Patient positioning refers to the careful placement of individuals in specific poses to ensure safety, comfort, and optimal outcomes during medical procedures and treatments․

1․1 Definition and Importance of Patient Positioning
Patient positioning is the strategic placement of individuals in specific poses to facilitate medical procedures, enhance accessibility, and ensure safety․ Proper positioning is vital for effective treatment, as it provides optimal access to surgical sites and minimizes risks of complications․ It also ensures patient comfort, preventing discomfort and long-term health issues․ Accurate positioning is critical in diagnostic imaging and surgical interventions, directly impacting the success of treatments․ Ensuring correct placement is a collaborative effort among healthcare professionals to achieve the best outcomes and efficiency․
1․2 Evolution of Patient Positioning Techniques
Patient positioning techniques have evolved significantly over time, driven by advancements in medical technology and a better understanding of patient needs․ Early methods focused on basic comfort and accessibility, while modern approaches integrate precision tools and imaging technologies․ The development of specialized tables, cushions, and immobilization devices has enhanced accuracy and safety․ Recent studies highlight innovations like advanced imaging guidance and real-time monitoring systems․ These improvements aim to minimize complications and optimize outcomes․ The evolution reflects a growing emphasis on patient-centric care, ensuring procedures are both effective and safe․ Continuous research and innovation are reshaping patient positioning, making it a cornerstone of modern healthcare practices․

Common Patient Positions
Common patient positions include supine, prone, Fowler’s, dorsal recumbent, lithotomy, Trendelenburg, and lateral, each serving specific purposes for comfort, accessibility, and procedural success․
2․1 Supine Position
The supine position involves the patient lying flat on their back, often with their arms at their sides or above their head․ This position is commonly used for general surgery, as it provides easy access to the abdominal and thoracic regions․ Additionally, it allows for straightforward endotracheal intubation and monitoring․ The supine position is ideal for procedures requiring minimal strain on the patient, such as cardiac surgeries or laparoscopic operations․ However, it may lead to respiratory challenges in patients with pre-existing conditions, necessitating careful monitoring by anesthesiologists․ Proper support, such as padding under the knees, is essential to prevent discomfort or long-term complications․
2․2 Prone Position
The prone position involves the patient lying flat on their stomach, with their head turned to one side and arms placed either above their head or alongside their body․ This position is commonly used in spinal surgeries to ensure proper alignment and access to the vertebrae․ It is also beneficial for patients with acute respiratory distress syndrome (ARDS), as it improves oxygenation by distributing lung secretions more evenly․ However, prone positioning requires careful monitoring to avoid complications such as pressure sores or nerve damage․ Proper padding and regular repositioning are essential to ensure patient comfort and safety during prolonged procedures․
2․3 Fowler’s Position
Fowler’s position is a semi-upright position where the patient is placed at a 45- to 60-degree angle, with their head elevated and knees slightly flexed․ This position is commonly used to improve respiratory function, as it allows the diaphragm to move more freely, enhancing lung expansion․ It is particularly beneficial for patients with breathing difficulties, such as those with heart or lung conditions․ Fowler’s position also aids in digestion and can reduce the risk of aspiration․ Variations include low Fowler’s (30-45 degrees) and high Fowler’s (60-90 degrees), each tailored to specific medical needs․ Proper support and padding are essential to ensure comfort and prevent strain during prolonged use․
2․4 Dorsal Recumbent Position
The dorsal recumbent position involves placing the patient on their back with legs elevated and supported, often using a wedge or stirrups․ This position is ideal for gynecological exams, urological procedures, and certain surgeries requiring access to the pelvic area․ It facilitates easy access for healthcare providers while maintaining patient comfort․ The legs are typically flexed at the hips and knees, with the feet secured to prevent movement․ This position also helps in managing postural drainage for respiratory conditions by allowing gravity to aid in mucus clearance․ Proper support and cushioning are crucial to avoid pressure points and ensure the patient remains comfortable throughout the procedure․
2․5 Lithotomy Position
The lithotomy position involves placing the patient on their back with legs elevated and supported by stirrups or a lithotomy pole․ This position is commonly used during gynecological, urological, and colorectal procedures to provide easy access to the pelvic area․ The patient’s hips are typically flexed, and the legs are separated, allowing healthcare providers to perform exams or surgeries efficiently․ Proper padding and support are essential to prevent discomfort and nerve damage; The lithotomy position can also be modified, such as the low or high lithotomy, depending on the procedure’s requirements․ It ensures optimal exposure while maintaining patient safety and comfort during medical interventions․
2․6 Trendelenburg Position
The Trendelenburg position involves tilting the patient in a supine position so that their head is lower than their pelvis, typically at an angle of 15–30 degrees․ This position is often used to improve oxygenation and venous return, particularly in critically ill patients․ It is also utilized during abdominal and gynecological surgeries to enhance access to pelvic organs․ The Trendelenburg position can help prevent the small intestine from obstructing the pelvic cavity, providing better surgical exposure․ However, prolonged use may lead to complications such as respiratory compromise or increased intracranial pressure․ Proper monitoring and adjustments are crucial to ensure patient safety and comfort during this positioning․
2․7 Lateral Position
The lateral position involves placing the patient on their side, either left or right, with the body aligned in a straight line from head to heels․ This position is often used for procedures requiring access to the spine, lungs, or kidneys․ The patient’s ears, shoulders, hips, and ankles should be aligned to maintain proper body alignment․ Supports such as pillows or pads are used to prevent pressure sores and ensure comfort․ The lateral position is beneficial for patients with respiratory issues, as it can improve lung expansion․ It is also commonly used in orthopedic and neurosurgical procedures․ Proper padding and continuous monitoring are essential to prevent complications such as nerve damage or skin breakdown․

Patient Positioning in Specific Medical Procedures
Patient positioning is crucial in procedures like spine surgery, radiotherapy, and orthopedic operations, ensuring accuracy, safety, and optimal outcomes while minimizing risks and complications for the patient․
3․1 Patient Positioning in Spine Surgery
Patient positioning in spine surgery is critical for ensuring proper alignment and access to the spinal structures․ The prone position is most commonly used, as it allows for optimal exposure of the posterior spine․ However, other positions, such as the supine or lateral decubitus, may be employed depending on the surgical approach and the region of the spine being operated on․ Accurate positioning is essential to minimize complications, such as nerve injury or poor visualization of the surgical site․ Surgeons and anesthesiologists collaborate to ensure the patient is positioned safely, with padding and supports used to maintain stability and prevent pressure sores․ Proper positioning also facilitates intraoperative imaging and reduces the risk of postoperative discomfort․
3․2 Positioning for Endotracheal Intubation
Proper positioning is critical for successful endotracheal intubation, a high-risk procedure requiring precise technique․ The patient is typically placed in the “sniffing” position, with the neck flexed and head extended, aligning the oral, pharyngeal, and laryngeal axes․ This position optimizes laryngoscopic view and facilitates tube placement․ Anesthesiologists must ensure the patient’s head and neck are correctly aligned to minimize complications, such as difficult laryngoscopy or airway trauma․ Adequate positioning enhances intubation success and patient safety, reducing the risk of procedural complications․
3․3 Cardiac PET Imaging and Patient Motion
Cardiac PET imaging is a diagnostic tool offering high accuracy for myocardial perfusion studies with minimal radiation exposure․ However, patient motion during scans can compromise image quality, leading to diagnostic challenges․ Motion artifacts may obscure vital details, reducing the reliability of results․ To mitigate this, patients are instructed to remain still and follow breathing guidelines․ Techniques such as respiratory gating and motion correction algorithms are employed to enhance image clarity․ Ensuring minimal patient movement is critical for accurate cardiac PET imaging, enabling precise diagnosis and effective treatment planning․ Proper positioning and patient compliance are essential to optimize imaging outcomes in cardiac PET procedures․
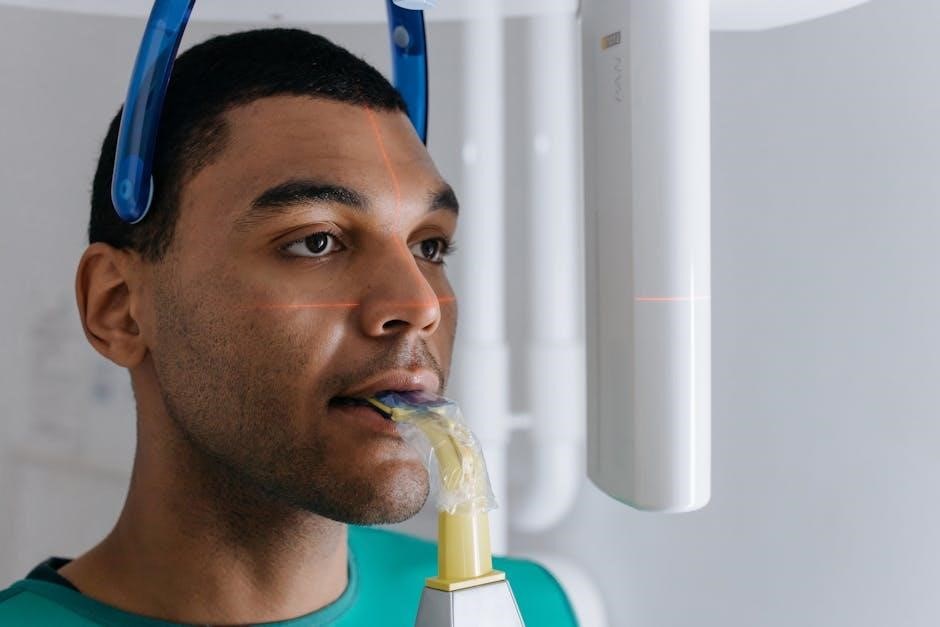
3․4 Radiotherapy Patient Positioning
Radiotherapy patient positioning is crucial for delivering precise radiation doses to target areas while minimizing exposure to healthy tissues․ Accurate positioning ensures treatment efficacy and reduces side effects․ Techniques like immobilization devices, such as masks or molds, are used to maintain consistency․ Imaging technologies, including CT and MRI, guide precise alignment․ Upright postures are sometimes preferred, as they reduce organ movement and setup time․ Innovations in positioning systems enhance reproducibility and comfort, improving overall patient outcomes․ Proper alignment and stability are critical for effective radiotherapy, ensuring the treatment’s success and safety․
3․5 Positioning in Orthopedic Surgery
Positioning in orthopedic surgery is critical to ensure proper alignment and access to joints or bones․ The supine position is commonly used for procedures like hip or knee replacements, while the prone position is often employed for spinal surgeries․ Lateral positioning is ideal for shoulder or hip surgeries, allowing easy access to the affected joint․ Proper positioning minimizes complications and enhances surgical precision․ Specialized tables and traction devices are utilized to maintain stability and alignment․ Collaboration between surgeons and anesthesiologists ensures optimal patient placement, balancing comfort and surgical needs․ Correct positioning is essential for successful outcomes, reducing the risk of nerve damage or improper healing;
3․6 Prone Positioning for Acute Respiratory Failure
Prone positioning is a critical intervention for patients with acute respiratory failure, particularly those with severe acute respiratory distress syndrome (ARDS)․ By placing the patient face down, it improves lung mechanics and oxygenation in 60-70% of cases․ This technique enhances ventilation-perfusion matching and reduces atelectasis․ While prone positioning significantly improves oxygenation, its impact on mortality remains uncertain․ Despite this, it has become a standard practice in intensive care units for mechanically ventilated patients with severe ARDS, supported by high-quality evidence․ Proper implementation requires careful patient selection and monitoring to minimize complications․ Collaboration between healthcare teams is essential to ensure safe and effective use of this technique․

Market Analysis and Trends
The global patient positioning systems market, valued at $1․17 billion in 2021, is projected to reach $1․71 billion by 2030, growing at a 4․5% CAGR․
4․1 Global Patient Positioning Systems Market Size

The global patient positioning systems market was valued at $1․17 billion in 2021․ This figure reflects the growing demand for advanced medical equipment and technologies that enhance patient care and procedural accuracy․ The market size is influenced by factors such as the increasing prevalence of chronic diseases, technological advancements, and the rising need for precise patient positioning in various medical procedures․ Additionally, the expansion of healthcare infrastructure in developing regions and the adoption of minimally invasive surgeries have contributed to market growth․ These trends underscore the critical role of patient positioning systems in modern healthcare, driving their global market value․
4․2 Growth Projections for Patient Positioning Systems
The global patient positioning systems market is projected to grow significantly, with a forecasted Compound Annual Growth Rate (CAGR) of 4․5% from 2021 to 2030․ This growth is driven by advancements in medical technology, an aging population, and increased demand for precise patient positioning in surgeries and radiotherapy․ The market is expected to reach $1․71 billion by 2030, up from $1․17 billion in 2021․ Factors such as the rising prevalence of chronic diseases, the adoption of minimally invasive procedures, and growing investments in healthcare infrastructure further fuel this expansion․ These projections highlight the critical role of patient positioning systems in modern healthcare․
4․3 Europe Radiotherapy Patient Positioning Market
The Europe radiotherapy patient positioning market is experiencing robust growth, driven by an aging population, rising cancer incidence, and technological advancements․ With a projected Compound Annual Growth Rate (CAGR) of 4․1%, the market is poised for significant expansion․ Key factors include increased investments in healthcare infrastructure, the adoption of advanced radiotherapy systems, and the growing demand for precise patient positioning to enhance treatment accuracy․ Additionally, the preference for upright patient positioning during radiotherapy, which reduces organ movement and improves outcomes, is gaining traction․ These trends underscore Europe’s role as a leader in adopting innovative patient positioning solutions for radiotherapy․

Patient Positioning and Safety
Patient positioning is critical for minimizing risks and ensuring safety․ Proper techniques reduce complications, while poor positioning can lead to discomfort, injury, or treatment delays․
5․1 Complications Arising from Inadequate Positioning
Inadequate patient positioning can lead to various complications, including nerve damage, skin breakdown, and respiratory issues․ Poor positioning may impair circulation, causing ischemia or pressure sores․ Additionally, it can restrict breathing, especially in prone or Trendelenburg positions, potentially leading to hypoxia․ In surgical settings, improper alignment may obstruct the surgeon’s access, increasing procedure time and risk of infection․ Furthermore, prolonged immobility in suboptimal positions can result in discomfort, pain, and long-term musculoskeletal issues․ Ensuring proper positioning is essential to prevent these complications and safeguard patient well-being․
5․2 Risks and Contraindications
Patient positioning carries inherent risks, particularly when contraindications are not considered․ Certain positions, such as prone or Trendelenburg, may worsen respiratory distress or exacerbate spinal instability․ Obesity, frailty, or pre-existing injuries can increase susceptibility to harm․ Additionally, prolonged immobility in compromising positions may lead to pressure sores or nerve compression․ Contraindications include conditions like recent fractures or severe arthritis, where movement could cause further damage․ It is critical to assess each patient’s unique condition and tailor positioning strategies to minimize risks and avoid complications․ Proper training and adherence to guidelines are essential to ensure safe and effective patient positioning․
5․3 Optimizing Patient Safety Through Proper Positioning

Optimizing patient safety through proper positioning involves careful planning and execution to minimize risks․ Proper positioning ensures patient comfort, prevents complications, and enhances procedural outcomes․ It is crucial to assess individual needs, considering factors like body weight, existing injuries, and medical conditions․ Using supportive devices, such as pillows, pads, and straps, can help maintain alignment and reduce pressure points․ Regular monitoring and adjustments during procedures are essential to prevent issues like nerve compression or respiratory distress․ A multidisciplinary approach, involving nurses, anesthesiologists, and surgeons, ensures comprehensive care․ By adhering to established guidelines and leveraging technology, healthcare providers can optimize patient safety, reducing the likelihood of adverse events and improving overall well-being․

Future Trends and Innovations
Future trends in patient positioning include the integration of AI, robotics, and real-time monitoring systems, enhancing precision and safety in medical procedures and treatments․
6․1 Advanced Techniques in Patient Positioning
Advanced techniques in patient positioning involve the use of cutting-edge technologies such as robotic systems and AI algorithms to optimize accuracy and minimize risks during procedures․ These innovations enable precise alignment and real-time adjustments, ensuring better surgical outcomes․ Additionally, virtual reality and augmented reality are being explored to enhance positioning accuracy․ Integration of these technologies with existing systems promises to revolutionize patient care, making procedures safer and more efficient․ Continuous research and development are driving these advancements, ensuring that patient positioning evolves to meet the demands of modern medicine․ The focus remains on improving both patient safety and procedural success rates․
6․2 Role of Technology in Patient Positioning Systems
Technology plays a pivotal role in modern patient positioning systems, enhancing accuracy and safety․ Advanced systems utilize robotic arms, AI algorithms, and real-time imaging tools like MRI and CT scans to ensure precise positioning․ These innovations reduce complications and improve procedural outcomes․ Automated adjustments and data analytics further streamline workflows, enabling healthcare providers to deliver personalized care․ The integration of technology into positioning systems has also led to reduced radiation exposure and faster setup times, particularly in radiotherapy․ As these technologies evolve, they promise to revolutionize patient positioning, making medical procedures more efficient and safer for patients worldwide․ The global market for such systems is growing rapidly, reflecting their increasing adoption․
